Heelal:
Hoe verder men keek
hoe groter het leek
Maar het bleek alras
hoe klein het ooit was
Jules Deelder
A Toronto doctor who received money from the sale of his father’s generic drug company has given $10-million toward improving the health of Canada’s indigenous people.
The man who heads the commission examining abuses at aboriginal residential schools says he understands the distrust of the medical system that would prompt native parents to pull their daughters out of chemotherapy over the objections of their doctors.
“And they may or may not have done the right thing,” he said. “But they did the thing that they thought was best based on all of the experience that they brought to the discussion.”
Those experiences, he said, include a history of coercion and oppression in which native children were forcibly removed from the homes of their parents to attend schools established, in part, to rid them of their culture.
Jules Deelder
OTTAWA — The Globe and Mail
A Toronto doctor who received money from the sale of his father’s generic drug company has given $10-million toward improving the health of Canada’s indigenous people.
The University of Toronto announced on Friday, National Aboriginal Day, that Michael Dan and his wife, Amira, made the donation to its Dalla Lana School of Public Health to create an institute that will study the health issues among the country’s aboriginal population.
“This is the single most important issue facing my generation, and if people like me don’t do something about it, then I wouldn’t be able to sleep well at night,” Dr. Dan said in a telephone call from Bosnia, where he was visiting his in-laws.
“The opportunity to do something about it is here,” he said. “The university is ready to tackle something like this.”
he institute created by the Dans will operate with the input of indigenous people and will bring together scholars in public health, medicine, nursing, social work, education, law, anthropology and many other disciplines. It will tackle a complex and difficult issue.
The life expectancy of First Nations people is five to seven years shorter than that of the general population. Among the Inuit, it is 15 years shorter. Indigenous newborns have a mortality rate that is 1.5 times that of babies in the rest of Canada, and they have more birth defects.
People living on reserves are 31 times more likely than other Canadians to contract tuberculosis. They are three to five times as likely to develop diabetes. They bear a disproportionate risk of traumatic injury. And their rates of infectious disease and suicide are significantly higher.
“If you look at it in totality, it’s completely overwhelming,” Dr. Dan said. “But I think it’s possible, working on a community-by-community basis, to just make a little dent in some of these big issues. You’ll never achieve anything unless you sit down with a community and ask, ‘What are your health problems, how can we help you?’”
The University of Toronto will host Canada’s first indigenous health conference later this year.
Medical system told to examine why aboriginal parents distrust it
TORONTO — The Globe and Mail
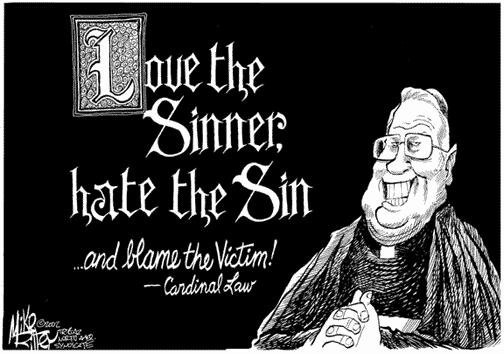
Murray Sinclair, the chair of the Indian Residential Schools Truth and Reconciliation Commission, said the recent moves by two sets of First Nations parents to discontinue the cancer drugs prescribed for their daughters should prompt the medical community to ask itself what it is doing wrong.
“It is very clear to me that a significant feature of the decision-making process that went into those parents’ decisions to do what they did was that they did not trust, and did not like, the way that the medical system was going to treat their children,” Judge Sinclair said on Thursday during a two-day conference on aboriginal health.
“And they may or may not have done the right thing,” he said. “But they did the thing that they thought was best based on all of the experience that they brought to the discussion.”
Those experiences, he said, include a history of coercion and oppression in which native children were forcibly removed from the homes of their parents to attend schools established, in part, to rid them of their culture.
So when the medical community asks the legal system to force parents to submit their children to treatments they do not support, “it now just generates more distrust,” Judge Sinclair said. “It is not for the doctors, in my view, to now go to the court and say to the court, you must compel these parents to let us do what we want to do to that child. It is, in fact, for the parents, I think, to be persuaded that what they are going to do will engage them in a way that’s appropriate.”
An Ontario judge ruled last week that a hospital cannot force an 11-year-old girl from the Six Nations of the Grand River community in southwestern Ontario to resume chemotherapy because the Constitution protects her mother’s right to treat the child with traditional aboriginal medicine.
Doctors at McMaster Children’s Hospital in Hamilton had said the girl, known publicly as J.J., had a better than 90 per cent chance of a cure if she was treated with the drugs. Without them, they said, she would die.
J.J.’s parents pulled her out of the chemo after just 10 days of the planned 32-day course of therapy, saying they rejected the “Western paradigm of medicine.” The doctors then asked the local child welfare agency to force the child from her family and back into hospital. When the child-welfare authorities refused, the doctors took them to court.
But Ontario Court Justice Gethin Edward rejected the doctors’ bid. The decision angered many Canadians, who argued that the child, and an 11-year-old girl at a different Ontario First Nation who was in a remarkably similar situation, were simply being allowed to die.
Chief Ava Hill of the Six Nations, who lauded the ruling in the hours after it was delivered, said Thursday it was the doctors who handled the situation badly by threatening to apprehend the child. “Why weren’t they opening their eyes to say, ‘Let’s talk about what other alternatives there are,’ including our traditional medicine.”
Hospital spokesmen now say the institution is open to combining aboriginal traditional medicine with the chemotherapy and they hope J.J. will come back for treatment.
Lisa Richardson, a clinician-teacher in the University of Toronto’s division of general internal medicine who is of Anishinaabe and European descent, said Canada has a long history of children being taken away from aboriginal people. That means forced apprehension is not a good approach in situations like this, she said.
“Health-care providers have to learn a new way to deal,” Dr. Richardson said. “They have to understand that their aboriginal patients are bringing either those personal experiences or those community experiences of the historical trauma with them.”
 |
| BRON |


















Geen opmerkingen:
Een reactie posten